The development of successful ‘smart insulin’ in glucose responsive ‘closed loop’ insulin delivery system is already taken into research basically to deliver insulin in response to increased glycemic levels, which may provide optimal glucose control with negligible patient’s effort and also tend in improving the quality of life in diabetic patients.
Diabetes Mellitus (DM) is a chronic life-threatening disease just like cancer or any other disease whose incidence has become doubled in recent years. In diabeties patients, the use of intensive insulin therapy was found to reduce long term vascular complications and some evidence also highlights the increased risk of both hyperglycemia and hypoglycemia. Islet transplantation has significantly increased over the past decade, yet there are issues of immunosuppressive drugs and the unavailability of adequate pancreatic donors. Nowadays, novel insulin analogues have improved pharmacokinetics profile corresponding to endogenous basal and prandial insulin secretion more strongly. However, despite advances in insulin formulations, external insulin infusion pumps, glucose control still remains a challenge. Patients with diabetes do not achieve their glycemic targets which, therefore become a major hurdle for the development of insulin therapy.
Diabetes, which causes uncontrollable increase in blood glucose levels, is globally one of the most prevalent chronic diseases. It is a metabolic disorder which either causes permanent lack of insulin production from the pancreas (type 1 diabetes) or a condition where the cells fail to respond to insulin due to dysfunction (type 2 diabetes) which later elevates the blood glucose levels. Insulin is a hormone which is synthesised and secreted from the pancreas to meditate the metabolic reaction involving glucose. In the absence of insulin, the cellular system cannot accurately convert carbohydrates such as sugars, starches, or other foods into energy which is used by the body. These factors in due course result in many complications, such as cardiovascular disease, chronic renal failure, retinal damage, nerve damage, and microvascular damage. According to the reports given by the World Health Organization (WHO), Around 180 million people globally are affected by diabetes and as estimated, the number will increase over 350 million by the year 2030. In the human body, insulin and glucagon are counter regulatory hormones that play a vital role in regulating blood glucose levels. Either excess or shortage of glucose in the blood is known as a metabolic disorder.
History reveals that diabetes emerged around 2000 B.C, which was discovered by Wells and Lawrence. The discovery of insulin and its functionality was in the year 1921, and continuous glucose monitoring was introduced in 1999. Despite many difficult situations, recent engineering is being focused on many advancements towards individual components that can be combined into closed loop systems that can facilitate a controlled blood glucose levels in a predetermined amount and time under defined conditions without any human input. Diabetic patients are recommended to check their blood glucose levels and take periodic insulin for better management of blood glucose levels. However, patients often do not follow the suggestion as per prescribed as there is a lot of pain, intense stress for repetitive blood collection and insulin shots. These complications lead to various severe diabetic problems like cardiovascular, kidney disease, stroke, blindness and nerve degeneration. In addition, insulin over treatment causes a sudden drop in blood glucose concentration which may cause seizures, unconsciousness and even death. Initiation of continuous glucose monitoring in the early 1960s was landmark which was led by the first production of hospital based commercial artificial pancreas. Intravenous sensing of glucose and insulin delivery combination was developed in the late 1970s. For many decades, automated closed loop insulin delivery also referred as an ‘Artificial Pancreas’ has been an important difficult goal, also now for researchers in treating diabetes. In the past 10 years, research into an artificial pancreas that is on the closed loop delivery system has gained significant interest and focus has been done on the subcutaneous route for glucose measurement and delivery. This will further help in advancing more towards interstitial glucose monitoring and thereby increasing the use of this combination.
This closed loop delivery system will perhaps happen gradually, and would have benefits like glycemic control, and thereby the ability to temporarily shut off of pump to overcome the situation like maintaining glucose levels between the meals and exercise. A plethora of biosensors have been developed which enables in providing diagnostic information regarding a patient’s health status. Many different types of sensors have been investigated and a 2010 review by Toghill and Compton gave a great insight into enzymatic and non-enzymatic electrochemical glucose sensing approaches studied over the past decades. Now, non-invasive spectroscopic methods for glucose detection have also been growing in popularity with Raman and Infrared Spectroscopy gaining particular attention. However, the main challenge that still remains is the creation of biosensors for daily use by patients in a personalised monitoring format. Recently, several reviews focusing on sensor integration developed into wearable platforms have been published. Therefore, a novel method which will be pain and stress -free in monitoring glucose levels and maintaining homeostasis accurately is highly desired in the management of uncontrolled diabetes. This article solely focuses on recent advances towards noninvasive and continuous glucose monitoring devices with a particular focus planned on monitoring glucose concentrations for diabetics.
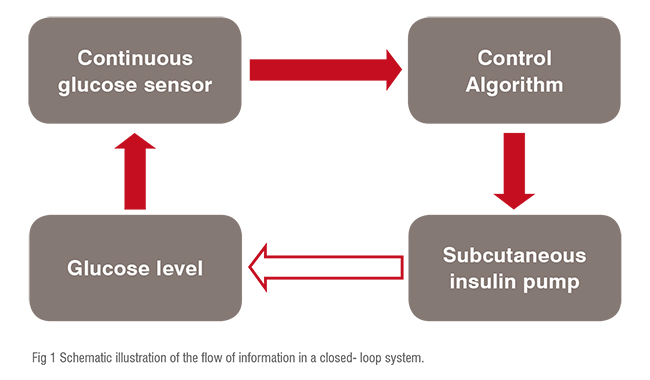
The information flows in a closed-loop system where the continuous glucose sensor sends control algorithm which pumps adequate insulin into the body to maintain the glycemic levels, it showned in figure 1.
Currently there is no artificial pancreas approved and available in the market. The artificial pancreas may contain functionally integrated components that will moreover continuously sense glucose levels, thereby determining appropriate insulin dosage and also delivering insulin in proper time. Several components related to artificial pancreas have been developed which includes, the use of glucose sensor and insulin pump which is linked via wireless communication system for adequate glucose monitoring and parental delivery of insulin in diabetic patients. Currently available intensive therapy has been found to vary in managing glycemic levels by the use of the closed-loop system. This helps in regulation of glucose levels in diabetic patients. Glucose levels are continuously monitored without any requirement of patient's input. Measuring glucose levels looked promising with minimum invasive methods for outpatient glucose monitoring. Existing commercially available sensors are directly inserted into the subcutaneous tissues that measures electric current, generated by the oxidation of glucose via the enzyme glucose oxidase. For the development of artificial pancreas; till date different types of the glucose sensors, along with four available types of insulin algorithms and insulin delivery systems are in the research phase. The ultimate focus is on the development of a combination of better glucose monitoring and insulin delivery technologies by way of an algorithm into an automatic closedloop system. This development results in the decrease in glycemic variability and fewer hypoglycemic conditions. Hence, the procedure is painless as compared to needle pricking to monitor glucose levels and deliver insulin for effective management of diabetes.
An ‘Artificial pancreas’ is a technology which stimulates the secretion of insulin in response to elevated glycemic levels. It is a closed-loop system which monitors the glucose levels in blood and triggers the insulin release to regulate and maintain glycemic variability without obstructions. It is considered to be a potential advance system in regulating glycemia and thus improving quality of life. A closed-loop system is a combination of glucose monitoring module and insulin release sensor.
Continuous monitoring of this glycemic level is basically enabled by blood-glucose tests and then accordingly adjusted insulin shots can lead to reduced use of artificial pancreas or closed-loop insulin delivery called as “Smart” insulin patch. ‘Smart’because it releases insulin according to the body’s need. This combines the use of glucose sensor which monitors glucose levels and insulin sensor which pumps insulin via the controlled algorithm as per the glucose readings. This system mimics the role of ? cells to regulate the blood glucose levels. However, gathering accurate signal feedback of the glucose level and thereby maintain the glycemic variability still remains an important challenge for such a device. A chemical approach such as use of insulin-loaded matrix in a glucose sensor with a relevant actuator could be beneficial in the closedloop system for the release of insulin. The changes remain to demonstrate a strategy which could manage both fast response of insulin administration along with tremendous biocompatibility.
Other modified applications for closed-loop insulin delivery include microneedles via transdermal route. Microneedles have been found to be versatile and researchers are now focusing on development of different microneedles based on metals or polymers comprising of an enzyme such as Glucose Oxidase (GOx) as sensor along with insulin. These have been known to passing small amount of insulin through microneedles via auxiliary pumping systems thus maintaining quantitative control and providing continuous delivery. In recent years, human skin has become very popular method for monitoring glucose. The Glucowatch was developed as a wearable device was initially brought to mark for noninvasive continuous monitoring glucose to measure glucose levels, but due to its limitation the product was removed from the market in 2008.
The concept of Microneedle was used for the development of a glucose sensing patch, since this approach can offer minimally invasive methods for biosensing. "The miniaturized device spans a total area of 6x6mm in which it contains 200 hollow microneedles (300micrometer in length with a 50x50 micrometer lumen). Three screen-printed electrodes were used for quantifying glucose concentrations in the interstitial fluid including a Pt- C working electrode covered with a layer of cross-linked bovine albumin serum and glucose oxidase. The sensing device was attached to the skin by an adhesive layer contouring the perimeter of the sensing pod. Detection was performed upon glucose diffusion into the microneedle array wherein GOx could react to produce hydrogen peroxide"1. This microneedle patch allows the patch to be in constant contact with the skin, providing permanent access to the interstitial fluid and thus enableing this device to operate continuously.
Due to this short length of the microneedle there is precise penetration for interstitial fluid sampling, thus it does not reach the dermis layer. Moreover, as the microneedle penetrate the skin, contamination by sweat is also avoided. Tests have shown that this device can operate successfully for upto 72hrs with only 17minutes lag time caused by the passive diffusion of analytes from the blood into the interstitial fluid matrix. Limitations such as clogging, distortion of the shape upon the penetration of the skin can affect the dynamics of the sampling. However, this novel device holds great potential for noninvasive continuous glucose monitoring. Scientist Zhi and his team further developed the technology by encapsulating the sensors in a thin film which gave the benefits of fast analyte transport through the device. This approach might be designed for pancreatic islet transplants which are known treatment procedure for Type 1 diabetic patients. Microneedles can be safe for maintaining artificial pancreas environment thus increasing the system reliability, decreasing the feeling of pain and also implementing a systematic closed-loop delivery system on insulin. The smart insulin patch could be a game changer as it can be placed anywhere on the body to detect increase in glucose level (Figure 2).
This article highlights the benefits of a closed-loop system and thereby encourages the developments of an artificial pancreas. The ideal medication would be the biological cure where the ? cells, which are damaged, could be replaced with healthier ones. The innovation of artificial pancreas could bridge the gap until a total cure is obtained. The majority of patients still struggle to achieve the optimal blood glucose levels; even with the sophisticated insulin pumps and continuous glucose monitoring devices. The artificial pancreas may become a more convenient and superior mode of insulin delivery. An intravascular device that can be implanted and which can sense glucose and deliver insulin to maintain optimum glycemic levels would be a safe, easy, pain-free and a reasonable method for the management of diabetes in near future.