The latest COVID-19 disease outbreak caused by novel corona virus, which is now officially known as SARS-CoV- 2 extreme acute respiratory syndrome, is a global public health pandemic. While the COVID-19 outbreak in Wuhan, China, was in December 2019, it spread to over 100 countries. This disease spread to more than 100 nations with more than 14, 50,343 confirmed cases, and more than confirmed 83,568 fatalities worldwide till 8 April 2020. However, as a consequence of the mandatory isolations / quarantines millions of people were affected by this disease. If COVID-19 is not efficiently regulated the spread of the virus, may potentially pose significant challenges to global health systems and have far-reaching consequences in the world economy.
There is a widespread panic around the world about COVID-19, caused by the novel Coronavirus. In late December 2019, China health Officials reported an outbreak of pneumonia of unknown origin in Wuhan, Hubei province. The World Health Organisation (WHO) originally called this disease "Novel Coronavirus-infected Pneumonia (NCIP) and this novel coronavirus was provisionally named 2019-nCoV. Novel, because it is new to humans, meaning that this specific virus is one that we have never seen before. The disease is potentially a case of zoonotic transmission that may occur through contact and respiratory route. Arrival of COVID-19 is disturbing as the human body lacks immunity against this virus, combined with its ability to spread and its relative lethality. The virus is spreading globally at an alarming late since its discovery and has been causing thousands of deaths and subsequently having an impact on our health systems and as well as economy. After China, it has spread subsequently to 37 other countries including Italy, United States, Japan, South Korea, Australia, Iran, France and India. The outbreak was declared as Pandemic and Public Health Emergency of International Concern on 11 March 2020, by WHO. As of 20 April 2020, there have been 2,319,066 confirmed cases of Corona spreading across 213 countries.
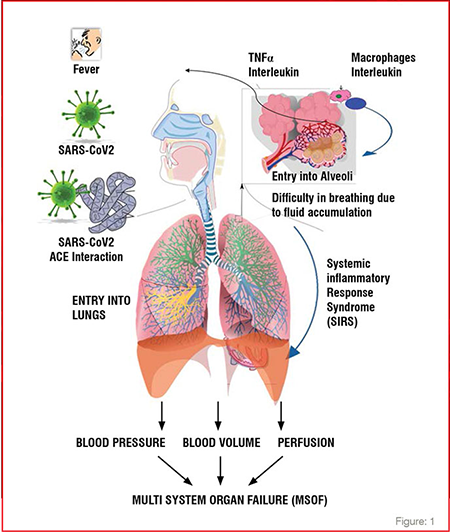
The incubation period of COVID-19 is assessed to be between 2 and 14 days, meaning the symptoms appear to develop within 14 days after coming in contact with someone with confirmed coronavirus. COVID-19 is mainly transmitted through droplets generated when an infected person coughs, sneezes, or exhales. Also, these droplets are too heavy to hang in the air, and quickly fall on floors or surfaces and one can be infected by breathing in the virus if he comes in proximity of someone who has COVID-19, or by touching a contaminated surface and then your eyes, nose or mouth and Corona viruses can also spread by aerosolisation as well. Clinical presentations of COVID-19 range from no symptoms (asymptomatic) to severe pneumonia. COVID-19 patients primarily show symptoms of fever, fatigue or myalgias and dry cough. Patients with severe illness may develop dyspnea and hypoxemia within a week after onset of the disease, which may quickly progress to acute respiratory distress syndrome (ARDS) or end-organ failure. Though majority of cases (almost 80per cent) are milder respiratory infections and pneumonias and the severe illness and death is more common among the elderly or the individuals with other comorbidities like diabetes, hypertension, smoking history, weak immune system or pre-existing lung disease. (Figure: 1)
SARS, MERS and COVID-19 are viral respiratory infections and belong to the common genome of a virus. Research has shown that SARS-CoV and MERSCoV originated in bats, and it is likely that SARS-CoV-2 did as well. SARSCoV then spread from infected civets to people, while MERS-CoV spreads from infected camels to people. However, the scientists are trying to determine how SARS-CoV-2 spread from an animal reservoir to people. The reproductive transmission number for COVID-19 is estimated by WHO is between range of 2 to 2.5 which is higher than SARS (1.7 to 1.9) and MERS (<1), clearly indicating that it has higher potential to spread. However, the fatality rate of novel coronavirus infection is estimated to be 2.3, which is lower than SARS (9.5 per cent) and much lower than MERS (34.4 per cent).
Countries around the world were in a state of panic about the spread and are still concerned that the magnitude of this pandemic cannot be taken lightly. India too took up the control measures as directed by WHO guidelines, first and foremost step taken up was traveler screening at airports, in order to curtail the geographic spread of infection. But it was effective for short mean incubation period. For larger incubation periods, travelerrs will not show symptoms. They will be healthy enough to travel and it becomes difficult to detect. Hence, a containment plan which mentions about non pharmaceutical intervention was declared. ‘Quarantine’ and ‘Isolation’ were the important contents of the containment plan. Quarantine refers to separation of individuals who are not yet ill but have been exposed to COVID-19 and thus have a potential to become ill. Isolation refers to separation of individuals who are ill, suspected, or confirmed COVID-19 cases. Doctors and nurses were provided with online training on management of COVID-19 patients. Tele- consultation facility was provided to ensure that all COVID- 19 patients should get uniform clinical care. Quarantine Facilities were set up. A meticulous surveillance system in line with contract tracing enabled to track the individuals who tried to avoid the surveillance and didn’t follow the quarantine measures.
Social Distancing measures were implemented to mitigate the impact and interrupt the human to human transmission chain as it can reduce the intensity of the spread and slow down the increase in the number of cases thereby helping the Healthcare system to prepare and cope with influx of the patients. Also, restrictions on mass gatherings were imposed in order to contain the virus. Social distancing at work places, measures for closure of schools and sanitisation of areas to limit the spread of transmission were adopted.
Lockdown was declared nationwide on 25 March 2020 in order to contain the spread and flatten the curve. But it was assured that all daily essentials will be provided to the citizens, while maintaining stringent safety norms.
The diagnostic tests for COVID-19 include molecular tests and serology tests. Detection is done by using two approaches- Whole Genome Sequencing and Real-Time Reverse Transcriptase PCR (RT-PCR). In earlier days of the outbreak, Sequencing was used for early documentation of this novel virus and its discovery and isolation. Currently, nearly all diagnostic testing is being done using RT-PCR. Abbott Testing kit known as ID NOW COVID was launched as game changer since it can deliver positive results in as little as five minutes and negative results within 13 minutes Various companies worldwide are manufacturing the coronavirus diagnostic test kits, which includes Glenmark Diagnostics, Cepheid, Bio fire Diagnostics, Meridian Biosciences. In India too Mylab became the first company to launch diagnostic kits. SD Biosensor and Altona Diagnostics in India have also got the approval for the same. The test is done on respiratory samples — nasopharyngeal and throat swab.
Currently, no antiviral medication is recommended, and treatment is directed at relieving the symptoms. Clinical management includes prevention of infection, control measures and supportive care, which includes supplemental oxygen therapy and ventilatory support system when required. NSAIDS like ibuprofen are being used currently for symptomatic reliefs. Zinc, Vitamin D and Vitamin C studies have shown to reduce the length of viral infections and respiratory and lung inflammations. The idea behind treating the symptoms is to prolong the patient’s life and help him to develop his immunity system and remove the infection. Though specific treatment for COVID-19 is still not yet available, but the positive aspect is that drugs are being tested and clinical trials are giving results. The WHO announced it has helped to launch four “mega trials'' against COVID-19 and these trials are focusing on drugs that can directly block SARS-CoV-2 – the virus strain that causes coronavirus COVID-19, from replicating inside the lungs. Some of the main drugs on whose trial we are looking forward are Remdesivir, Lopinavir/ Ritonavir, Chloroquine and Hydroxychloroquine.
Remdesivir is an intravenous antiviral drug which is under study and has shown some positive changes in COVID-19 patients, but large trials are still needed. Combination of Lopinavir and Ritonavir is currently used to treat multiple sclerosis, thereby enhancing the body’s natural defense system against COVID-19. Chloroquine and Hydroxychloroquine can block the viruses and prevent infection, but still large trials are needed in collaboration with WHO. The studies have demonstrated that chloroquine phosphate inhibits SARS-CoV-2 and there have been studies to show that hydroxychloroquine sulfate inhibits SARSCoV-2 in vitro. Among those treated for COVID-19, Azithromycin is also believed to relieve the symptoms. In parallel to this, the combination of hydroxychloroquine and azithromycin had been evaluated in invitro studies on SARS-CoV-2 infected cells and showed that there was a considerable synergy of these two products if they are used at doses which are suitable in doses required for human body. As per Monash university study in Australia, a single dose of Ivermectin can stop the growth of Corona virus growth in cell culture within two days and has been suggested for clinical trials.
Two other kinds of treatments are also being explored in trials and these work in a different way. The first is passive immunization- that is the transfer or the transfusion of protective antibodies from someone who has recovered from COVID-19 to someone who is susceptible or at risk of catching COVID-19. This is also called as “Convalescent Sera.” Or the Plasma Therapy. Plasma Therapy has shown some positive results recently in treating the patients of COVID-19. Another method of treatment under study is blocking the part of the immune system which is reacting highly to the COVIDinfection.
The sad part is that this new Coronavirus appears to spread much faster than SARS. So, a virus that spreads easily presents a huge Public Health Challenge in designing a system that can efficiently contain it. Also, the primary risk assessment based on its epidemiological characteristics is that everyone is susceptible, and it is still not known about neutralizing and developing the immunity post infection. Individuals at higher risk for severe disease and death include old age individuals and those with underlying conditions of diabetes, hypertension, chronic respiratory illness and cancer. Understanding the COV infection among healthcare workers is one more aspect to be considered in risk assessment. It is important for not only the characterisation of viral transmission but also for preventing the future infection in healthcare workers and reducing the secondary infection in the health care setups. According to an estimate, India has a shortage of about 6 lakh doctors and near about 20 lakh nurses, and an even bigger number of supporting medical staff. This means losing even a single doctor or nurse or any supporting staff, due to lack of protective equipment or not following the standard operating procedure (SOP) in handling COVID-19 cases is a cost that India cannot afford to bear. Another risk factor that cannot be ignored is that a seasonal cycle to the Coronavirus epidemic is possible meaning that there is risk factor of ramping up the corona infection again from severe weather and climate change. Also, due to lockdown and people staying inside the houses there has come evidences of decreased level of Vitamin D deficiency and this can further reduce the immunity of the body and the person is at high risk of catching respiratory infections.
Despite India's proactive and swift move to contain this COVID-19 steps, there have been challenges in its way of fighting corona. Key concerns are the country's high population density, overburdened public health system, high prevalence of non-communicable diseases (NCDs), a smaller number of testing laboratories, and inadequate number of hospital beds, ventilators and ICU facilities. The absence of widespread testing is causing actual count to appear “statistically invisible”. Laboratory diagnostic capacity weakness at national and community levels of the Healthcare System in India can greatly reduce the effectiveness of outbreak containment. Hence, timely and accurate laboratory testing of specimens from cases under investigation is an essential part of the management of COVID-19. Social distancing in a densely populated Indian population is coming up as a risk factor. The houses in slum areas of India are so congested that people cannot follow social distance norms as recommended by the doctors. In Mumbai, seventy-one people have tested positive for coronavirus in Dharavi, Asia’s biggest slum. Lack of sanitation and an adequate sewage disposal system is also coming up a hurdle to contain the virus.
COVID-19 is not the first, nor will it be the last among rapidly spreading pandemics of high impact to cause health disruption and deaths. Pandemics are emerging at higher frequency and it is becoming difficult to contain because of population growth, economic integration, urbanisation, migration, climate changes and faster travels. A comprehensive strategy, including surveillance, diagnostics, clinical treatment, research, and development of vaccines and drugs, is urgently needed to win the battle against COVID-19 and other infectious diseases. The good part is that only after a few weeks of the discovery and isolation of SARS-CoV2, vaccine development started by scientists across the world. But failure is possible. There is no sure shot guarantee that a vaccine will develop within a short time period and even if it gets developed, it has to go under test for safety and efficiency. Artificial Intelligence and Data analytics can play an important role in modern genome sequencing methods. There is a need to create artificial intelligence (AI) programs and make it available to scientists to improve healthcare vastly. A greater understanding of these phenomena can empower the community to respond far more rapidly to such viral attacks. This approach can help to recognise any deviations before it reaches epidemic proportions. Global cooperation, collaboration and investment are necessary to ensure a safer future. We need to implement a multi-sectoral dimensional approach in managing the problem of global pandemic diseases that includes governments, industry, financial systems, academia, international organisations and civil society, everyone having responsibilities towards building a global public health security.